The longest life expectancy makes hemophiliacs susceptible to diseases not related to haemophilia and belonging to the general population as cerebro-cardiovascular pathologies and malignacies. Predictable is also that the younger patients, children and adolescents, suffer from disorders caused by well-being: obesity, metabolic syndrome, abnormal glucose tolerance.
In severe elderly hemophiliacs chronic arthropathy is the most frequent cause of falls and bone fractures aggravated by osteoporosis. These accidents imply a significant increase in major orthopedic surgery, particularly oriented to arthroplasty, including revisions of previously implanted prostheses. These interventions become more complex in hemophiliacs with inhibitors due to the increased bleeding risk and the costs they entail.
One of the emerging problems in major orthopedic surgery in elderly hemophiliacs is the risk of venous thromboembolism so far minimized.
The legitimate question arises whether venous thromboprophylaxis is mandatory in these cases. A scheme of venous thromboprophylaxis in hemophiliacs undergoing major orthopedic surgery suggests the administration of low molecular weight heparin subcutaneously 12-24 hours after intervention, continuing for at least 4 weeks or until mobilization. Venous thromboprophylaxis with elastic stockings and intermittent pneumatic compression is indicated in patients with inhibitor, early mobilization in arthroscopic procedures.
Literature reports that arterial hypertension is more prevalent in hemophiliacs than in males of the general population. It has been hypothesized that the phenomenon may be related to intensive replacement treatments, renal complications secondary to combined antiretroviral therapy or to repeated use of antifibrinolytics due to renal cortical necrosis.
Whether severe haemophilia protects against coronary ischemic events and atherosclerosis because of the congenital defect requires solid proofs. A lower incidence of mortality from cardiac ischemic events in hemophiliacs is reported than in the general male population, while atrial fibrillation appears to be as prevalent as in the non-haemophilic population: 3.4% in subjects over the age of 60. These data need specific recommendations on antithrombotic and anticoagulant treatments. Antithrombotic prophylaxis secondary to myocardial infarction with ASA 100 mg/day requires the anti-hemorrhagic protection with low doses of factor VIII/factor IX (FVIII/FIX) concentrates on alternate days. The use of non-medicated stents over medicated ones is preferable as it limits the association of ASA with clopidogrel or prasugrel to one month.
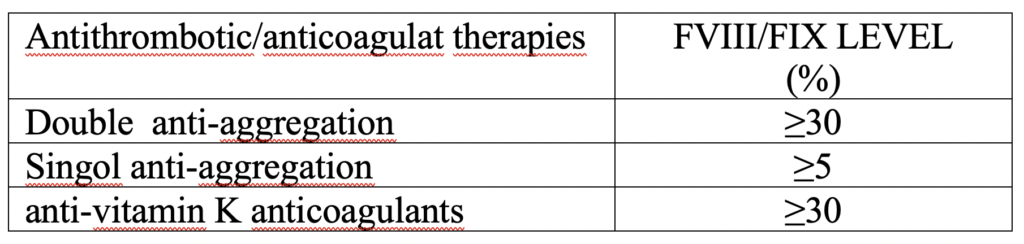
The blood levels (“trough level”) of the FVIII/FIX are specified below for antihemorrhagic prophylaxis associated with antithrombotic/anticoagulant therapies.
Attention must be kept to the risk of gastrointestinal hemorrhage always lurking with these specific treatments.
A dramatic reduction in mortality in HCV or HIV infection/coinfection is due to direct antiviral drugs for chronic hepatitis C and combination of antiretroviral treatment for HIV-infected persons. However, side effects have been observed secondary to the use of antiretroviral drugs such as metabolic syndrome, diabetes, nephrotic syndrome and cardiovascular diseases with a 26%/year increase in the relative risk of myocardial infarction.
In elderly hemophiliacs, attention is focused on the prevalence of malingnancies. As in the case of cardiovascular diseases, protection by the congenital defect has been hypothesized, for which the physiological state of anticoagulation would reduce tumor growth and implantation metastases. An Italian study showed that virus-related forms of cancer were significantly prevalent in severe hemophiliacs compared to moderate/mild ones, where related non-virus forms prevail (P = 0.0004). Furthermore the standard mortality rate was lower for the related non-virus cancer (SMR = 0.3), so that the mortality rate from virus-related cancer is higher in severe hemophiliacs. Supporting the above hypothesis, the mortality rate for non-virus related neoplastic forms decreases in severe hemophiliacs. Bleeding is described in chemotherapy (14%) and radiotherapy (19%).
It has been reported that the depressive state is more frequent in elderly hemophiliacs than in non-haemophilic males, which causes a worsening of the quality of life. Depressive state was also detected in elderly hemophilic with higher severity inhibitor compared to younger hemophilic with inhibitor.
A recent study “showed that obesity, hypertention and metabolic syndrome are frequent problems in young patients, especially in those over 18 years with arthropathy. Early prevention and management of overweight, obesity and their sequelae must be addressed in clinical practice in order to maximize the overall health of haemophiliacs. Therefore, assessment of cardiovascular and metabolic risk factors, beginning from early childhood, is crucial for this specific population.”.
The evaluation of comorbidities not strictly related to haemophilia requires particular attention in all age groups: from adolescence to adulthood and elderly age. Multispecialistic and integrated assistance to patients with haemophilia must include internists, geriatricians and general practitioners so that patients can be considered globally, focusing specific attention to the prescription of drugs.
Suggested readings
Konkle BA, Kessler C, Aledort L, Andersen J, Fogarty P, Kouides P, Quon D, Ragni M, Zakarija A, Ewenstein B. Emerging clinical concerns in the ageing haemophilia patient. Haemophilia. 2009 Nov;15(6):1197-209
Siboni SM, Mannucci PM, Gringeri A, Franchini M, Tagliaferri A, Ferretti M, Tradati FC, Santagostino E, von Mackensen S; Italian Association of Haemophilia Centres (AICE). Health status and quality of life of elderly persons with severe hemophilia born before the advent of modern replacement therapy. J Thromb Haemost. 2009 May;7(5):780-6.
Raza S, Kale G, Kim D, Akbar SA, Holm L, Naidzionak U, Hossain AM, Dong X, Doll DC, Freter CE, Hopkins T. Thromboprophylaxis and incidence of venous thromboembolism in patients with hemophilia A or B Who underwent high-risk orthopedic surgeries. Clin Appl Thromb Hemost. 2016 Mar;22(2):161-5.
Koo JR1, Lee YK, Kim YS, Cho WY, Kim HK, Won NH. Acute renal cortical necrosis caused by an antifibrinolytic drug (tranexamic acid). Nephrol Dial Transplant. 1999 Mar;14(3):750-2.
Fransen van de Putte DE, Fischer K, Makris M, Tait RC, Collins PW, Meijer K, Roosendaal G, Chowdary P, Schutgens RE, Mauser-Bunschoten EP. Increased prevalence of hypertension in haemophilia patients. Thromb Haemost. 2012 Oct;108(4):750-5.
Schutgens REG, Voskuil M, Mauser-Bunschoten EP. Management of cardiovascular disease in aging persons with haemophilia. Haemostasiologie 2017 Aug 7; 37 (3): 196-201.
Biere-Rafi S, Zwiers M, Peters M, van der Meer J, Rosendaal FR, Büller HR, Kamphuisen PW. The effect of haemophilia and von Willebrand disease on arterial thrombosis: a systematic review. Neth J Med 2010; 68: 207–214.
Tuinenburg A, Mauser-Bunschoten EP, Verhaar MC, Biesma DH, Schutgens RE. Cardiovascular disease in patients with hemophilia. J Thromb Hemost 2009; 7: 247–254. J Thromb Haemost. 2009 Feb;7(2):247-54.
Schutgens RE, Klamroth R, Pabinger I, Malerba M, Dolan G; ADVANCE working group. Atrial fibrillation in patients with haemophilia: a cross-sectional evaluation in Europe. Haemophilia 2014; 20: 682.
Mannucci PM, Schutgens RE, Santagostino E, Mauser-Bunschoten EP. How I treat age-related morbidities in elderly persons with hemophilia. Blood 2009; 114: 5256–5263.
Coppola A, Tagliaferri A, Franchini M. The management of cardiovascular diseases in patients with hemophilia. Semin Thromb Hemost. 2010 Feb;36(1):91-102.
Rumi MG, Di Marco V, Colombo M. Management of HCV-Related Liver Disease in Hemophilia and Thalassemia. Semin Liver Dis 2018; 38: 112–120.
Currier JS, Lundgren JD, Carr A, Klein D, Sabin CA, Sax PE, Schouten JT, Smieja M; Working Group 2. Epidemiological evidence for cardiovascular disease in HIV-infected patients and relationship to highly active antiretroviral therapy. Circulation 2008; 118: e29–35.
Tagliaferri A, Di Perna C, Santoro C, Schinco P, Santoro R, Rossetti G, Coppola A, Morfini M, Franchini M; Italian Association of Hemophilia Centers. Cancers in patients with hemophilia: a retrospective study from the Italian Association of Hemophilia Centers.
Yıldız M, Özdemir N, Önal H, Koç B, Eliuz Tipici B, Zülfikar B. Evaluation of Unfavorable Cardiovascular and Metabolic Risk Factors in Children and Young Adults with Haemophilia. J Clin Res Pediatr Endocrinol. 2019 May 28;11(2):173-180.
Mannucci PM. Aging with Hemophilia: The Challenge of Appropriate Drug Prescription. Mediterr J Hematol Infect Dis. 2019 Sep 1;11(1):e2019056.



